In this rapidly evolving digital age, technology has emerged as a transformative force in virtually all aspects of life, including healthcare.
In this rapidly evolving digital age, technology has emerged as a transformative force in virtually all aspects of life, including healthcare.
Telemedicine, the practice of leveraging telecommunications technology (audio/video conferencing, IoT devices, wearables, etc.) to remotely deliver healthcare services, has been a game-changer in the healthcare industry in recent years.
Telemedicine has bridged the gap between healthcare providers and patients like never before, allowing patients to accept medical care without having to travel to a hospital or a doctor’s office. In particular, telemedicine can be a valuable tool for patients who live in rural or underserved areas and those who have difficulty traveling.
This article will discuss how to set up a telemedicine service, and we will cover the following topics:
- Understanding telemedicine basics
- Overcoming challenges in setting up telemedicine
- Planning and setting up telemedicine services
- Ensuring data security and privacy
- Designing an efficient telemedicine workflow and patient experience
- Training your staff to make the most of the telemedicine solution
Whether you are a healthcare professional looking to improve your services or an entrepreneur seeking to jump into the lucrative telemedicine landscape, this article can serve as your guide to navigate the ever-evolving field of telemedicine.
Let’s delve into this guide right away.
Understanding The Basics of Telemedicine
Different Types of Telemedicine Services
Thanks to the advancements in technology, there are now many different types of telemedicine services catering to various medical needs.
However, despite the many different types available in the market, they can generally be divided into just four main categories:
- Synchronous telemedicine: this form of telemedicine involves real-time communication between a healthcare provider and a patient. For example, real-time virtual consultation via video conferencing. This type of telemedicine is often used for consultations, treatment planning, and remote diagnosis. Also known as real-time telemedicine.
- Asynchronous telemedicine: is a type of telemedicine in which the communication doesn’t happen in real time. In this type, medical data (diagnostic reports, x-ray photos, images, videos, etc.) is captured or sent by the patient and stored securely. Then this data can be forwarded to healthcare professionals for review at a later time. Asynchronous telemedicine is often used for chronic disease management, patient education, or to assist Remote Patient Monitoring (RPM.)
- Remote Patient Monitoring: RPM is the use of medical devices, wearables, and IoT devices, among other technologies, to monitor patients’ health data and vital signs remotely. RPM allows healthcare providers to continuously monitor patients’ conditions, and is especially useful in chronic illness management.
- Mobile Health (mHealth): this type of telemedicine utilizes mobile apps (and typically in combination with wearable devices) to allow patients to access healthcare services, receive information, and manage their treatment from their smartphones.
Before we delve further into how to set up your telemedicine service, first, you’ll need to decide what type of telemedicine service you will provide. We will explore more about this later when we discuss the planning process.
Overcoming Challenges in Setting Up Telemedicine
Despite the rapid growth and evolution of the telemedicine field, there are a number of challenges to consider before starting a telemedicine service. In this section, we will discuss these challenges and how to tackle them.
1. Regulatory and legal hurdles
The healthcare/medical industry in most countries is subject to complex, strict, and evolving regulations, and these regulations can widely vary from state to state and country to country.
Before starting a telehealth business, you must carefully navigate the applicable data privacy regulations, licensing requirements, healthcare privacy guidelines in your respective location, and so on. All of these can be resource-intensive and time-consuming.
2. Technology integration
Integrating your telemedicine solution with existing healthcare systems (i.e., Electronic Health Records/EHRs) can be very challenging in practice, and yet these integrations are crucial for efficient data exchange to facilitate patient care.
To tackle this issue, choose solutions (i.e., video conferencing software) that offer seamless integration and compatibility with the existing healthcare system.
3. User adoption and acceptance
When introducing telemedicine, you may face resistance from both healthcare providers and patients. Resistance to change is natural, so the telemedicine business must be effective in establishing trust and rapport.
To ensure widespread adoption, it’s also critical to educate users about the benefits and convenience of telemedicine.
4. Reimbursement and insurance coverage
There may be hurdles in getting telemedicine services reimbursed by insurance companies, with the varying reimbursement policies across payers and regions.
Entrepreneurs should closely work with credible insurance companies to get their telemedicine services covered, which may involve providing comprehensive documentation about the product. Also, it’s crucial to stay up-to-date on the latest changes in the reimbursement policies.
Another consideration is to try positioning your telemedicine service as an additional service to complement traditional in-person healthcare. Insurers may be more willing to cover telemedicine when it’s integrated with existing and more established healthcare services.
5. Digital divide
Even now, in 2024, there are still wide disparities in high-speed internet access and technological literacy, which may pose challenges for underserved populations.
To bridge this digital divide, entrepreneurs may want to develop and launch targeted outreach and education to raise awareness about telemedicine among underserved communities.
Collaboration with non-profits and local healthcare providers to reach marginalized populations can also help identify and target specific needs (i.e., accessible, low-cost internet) within the community.
Technology Requirements for Telemedicine Service
In order to provide a smooth, reliable, and secure telemedicine service, it’s critical to have an adequate technology infrastructure in place.
An ideal telemedicine platform should meet a number of technology requirements, including:
- Internet connectivity and bandwidth: High-speed and reliable internet bandwidth is crucial to ensure uninterrupted data transmission, especially during audio/video conferencing.
- Secure data transmission and encryption: protection of patient data privacy is critical in telemedicine. Implement robust encryption measures to secure all data transmissions during telemedicine consultations. Use secure file transfer methods and strict access control to prevent unauthorized access to sensitive medical information.
- Hardware and software requirements:
-
- A device with adequate processing power, storage capacity, and memory capabilities to support the telemedicine solution
- Decent-quality camera (i.e., webcam), microphone, and speaker to ensure clear video and audio communication. External video/audio equipment like external webcams and headsets can enhance the experience.
- Software should support real-time video conferencing, secure messaging, and secure data storage/encryption functionalities.
Planning and Setting Up a Telemedicine Service
In this section, we will discuss the key steps involved in setting up your telemedicine service. Yet, before the actual setup, it’s crucial to lay a solid foundation for the telemedicine service by defining clear objectives, identifying the target audience, and establishing comprehensive policies and protocols.
1. Defining Telemedicine Objectives
We’ll start by discussing the importance of outlining the objectives and goals of the telemedicine service.
It’s important to have clear, specific, and realistic (achievable) objectives so you can design and set up the telemedicine service according to these objectives.
Some common objectives for a telemedicine service include:
- Enhancing accessibility: for example, improving access to healthcare services for patients in rural areas or who have limited mobility.
- Increasing efficiency: streamlining healthcare delivery in one way or another, like reducing wait times, optimizing healthcare resource utilization, etc.
- Improving patient engagement: offering a user-friendly and convenient platform to enhance patient engagement during consultations.
- Delivering specialized care: utilizing telemedicine to provide specialized treatments or care programs that are otherwise impossible to deliver with traditional means.
2. Identifying Target Patient Population
Once you’ve identified your objectives, the next crucial step is to identify the right patient population that aligns with these objectives.
In short, you should answer the question,“Who are you trying to reach with your telemedicine service?” by considering the following factors:
- Geographical location: determine where your telemedicine service will be provided. Make sure to consider the provider’s capabilities and potential licensure issues.
- Medical conditions: what medical conditions can be more effectively managed through your telemedicine service?
- Demographics: the demographics of the target patient population, including age, gender, occupation, specific health needs, etc.
3. Establishing Telemedicine Policies and Protocols
To ensure seamless and secure delivery of healthcare services via telemedicine, according to your objectives, it’s important to establish the right policies and protocol. They will also help to ensure that your telemedicine service is compliant with the applicable laws and regulations.
You should establish policies and protocols for at least:
- Data privacy and security: develop robust data security policies to safeguard patient data. You should consider applicable data privacy regulations like HIPAA when developing your security protocols/policies.
- Informed consent: make sure to define and communicate a clear informed consent process/ The consent should inform patients of the scope of the telemedicine service, limitations, and potential risks.
- Emergency procedures: establish and communicate clear protocols for handling emergencies during virtual telemedicine consultations. This should include guidelines for escalation, and referrals to traditional in-person treatment if needed.
Selecting The Right Telemedicine Platform
While there is the option to build your telemedicine solution from scratch, our recommendation is to use a ready-made telemedicine platform so you can minimize development time while ensuring reliability.
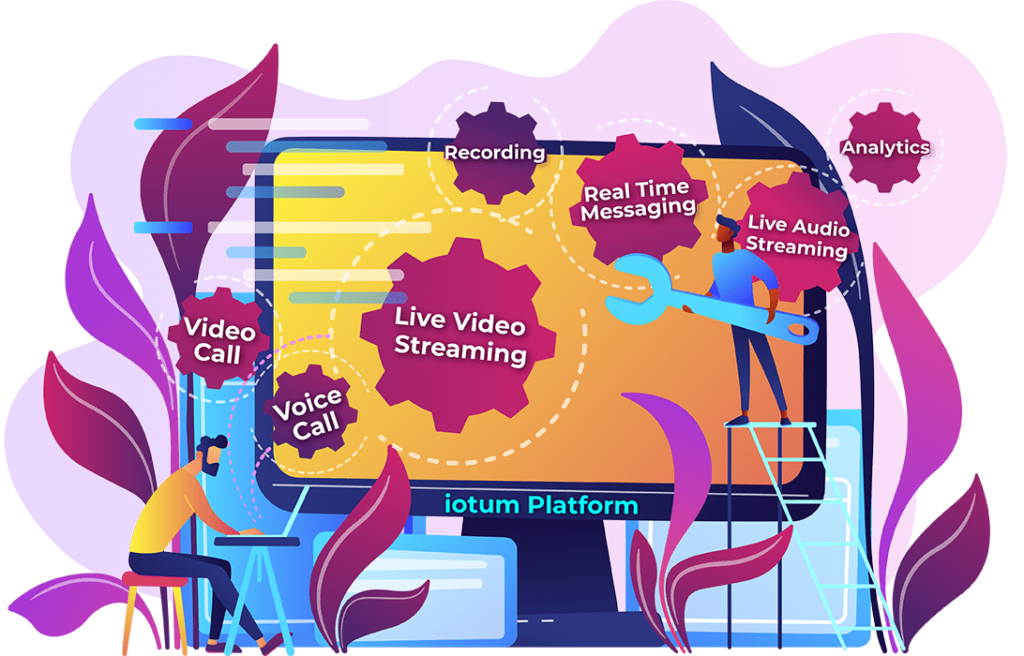
Iotum offers a video conferencing API that is tailored for telemedicine, offering a reliable, secure, and scalable video conferencing platform for telemedicine.
Iotum also offers a variety of features that can make setting up your telemedicine service more seamless, effective, and efficient, such as:
- High-quality video and audio: Iotum’s video conferencing APi offers crystal-clear audio and video quality, with adaptive bitrate ensuring the quality remains high even during low internet bandwidth.
- Secure and compliant: the Iotum telehealth video conferencing solution and API has a robust data security infrastructure to ensure patient data confidentiality and compliance with relevant healthcare regulations (i.e., HIPAA.)
- Ease of use: Iotum is designed to be easy to set up and use by both healthcare providers and patients
- Customization options: Iotum allows customization (including branding) and a wide range of integrations with existing healthcare systems to enhance efficiency and streamline workflows.
- Features for telemedicine: Iotum offers a variety of specific features designed for telemedicine, such as the functionality to share medical records.
Ensuring Optimal Telemedicine Workflow and Patient Experience
Ensuring a well-designed telemedicine workflow and positive patient experience is paramount to delivering quality virtual healthcare services.
In this section, we will discuss how.
1. Designing an efficient telemedicine workflow
Consider the following steps to ensure an efficient telemedicine workflow:
- Refer back to the objectives: remind yourself about what you hope to achieve with the telemedicine service. The idea is to design the workflow that will help you achieve these objectives.
- Identify the key steps: identify the steps that both healthcare providers and patients need to take to complete the telemedicine activity (i.e., a virtual consultation.) List these key steps so you can start to map out the workflow.
- Visualize the workflow: use a process-mapping tool to visualize the workflow. Doing so will help you identify any potential inefficiencies or bottlenecks in the workflow.
- Get feedback: once you’ve designed a workflow draft, get feedback from your staff, healthcare providers, and patients.
- Optimize the workflow: based on the feedback you’ve gathered, optimize the workflow to make sure it is intuitive, easy to follow, and as efficient as possible.
2. Designing a patient onboarding and consent process
Smooth patient onboarding and consent process is critical for any telemedicine workflow in two ways. First, it is essential to establish trust and provide a positive telemedicine experience. Second, it ensures compliance with relevant regulations.
Here are some tips you can consider:
- Provide clear and concise information: provide patients with comprehensive information that includes the benefits of the telemedicine service, any potential risks, and the patient’s rights and responsibilities.
- Use plain language: make sure the information provided is easy to understand. Avoid using overly complex medical jargon or technical terms.
- Collect and document patient consent: design the system so that you will always get patient consent before conducting any telemedicine appointment. The consent should include the patient’s understanding of the risks and benefits of the telemedicine service in question and should be well documented.
3. Scheduling and conducting telemedicine appointments
The core of the telemedicine workflow. This process should be designed to ensure convenience for both patients and healthcare providers while also ensuring data privacy and confidentiality.
Here are some key considerations:
- Use a secure platform: using a secure telemedicine platform like Iotum will help you ensure compliance and protect patient privacy and confidentiality.
- Provide clear instructions: provide patients with clear instructions on how to connect and use the telemedicine platform. This will help ensure the appointment starts on time, runs smoothly, and finishes as scheduled.
- Be prepared for technical problems: be prepared to troubleshoot any technical problems. Offer technical support to patients to address any platform-related or connectivity problems they may encounter before or during telemedicine appointments. If necessary, be prepared to reschedule the appointment.
- Appointment reminders: to make sure appointments start on time and to minimize no-shows, send appointment reminders via SMS or email.
4. Post-appointment follow-ups and patient feedback
Post-appointment activities ensure the patients are satisfied with the telemedicine service and help you make continuous improvement;Consider:
- Providing post-consultation instructions: provide patients with clear post-appointment instructions, including treatment plans, prescribed medications, follow-up recommendations, etc.
- Patient satisfaction survey: send patients a survey after their telemedicine appointment to gather feedback on their experience. This will allow you to identify areas for improvement.
- Quality improvement initiatives: use the collected feedback to optimize the workflow, technology, or patient education materials to enhance the telemedicine experience over time.
- Follow-up care: schedule follow-up telemedicine appointments when needed to ensure continuity of care and to improve patient engagement throughout their treatment.
Training Your Staff for Telemedicine
You’ve properly set up the telemedicine platform, but training your staff to use the platform effectively is crucial to ensure optimal healthcare service delivery.
Here are some tips you can use:
1. Start with familiarization
Make sure your staff understands the basics of telemedicine, its benefits, and its role in providing accessibility and enhancing patient care. Create awareness through emails, presentations, and team meetings to build engagement and excitement.
Also, train them on how to use the telemedicine video conferencing platform, how to protect patient privacy, and how to document each telemedicine consultation properly. If possible, offer hands-on training sessions so they can practice and explore using the telemedicine platform in a safe environment.
2. Use a variety of training sessions
Use a variety of training methods to accommodate those with different learning styles or experiences. This could include traditional lectures, online training, demonstrations, and role-playing, among others.
Especially encourage role-playing sessions where staff members can take turns acting as both patients and healthcare providers. This training method is effective in improving staff’s empathy and virtual communication skills.
3. Focus on patient communication
Your training should emphasize the importance of improving communication quality during virtual consultations.
Train staff members to maintain clear, empathetic, and concise communication, including how to incorporate non-verbal cues during virtual communications.
Regularly remind them about the importance of empathy and sensitivity in healthcare service, as patients may feel more vulnerable during virtual telemedicine sessions. Train your staff to improve attentiveness and active listening.
4. Address privacy and security
Emphasize the importance of patient data privacy and security during virtual consultations or any telemedicine interactions. Train your staff on the best practices in handling sensitive information and the importance of staying compliant with relevant privacy regulations (I.e., HIPAA).
5. Prepare for technical challenges
Anticipate the technical challenges your staff may face, and equip your staff with the tools and knowledge necessary to troubleshoot these technical issues. Provide your staff with a dedicated IT support contact and resources to help address more complex technical problems.
6. Celebrate milestones and achievements
Acknowledge and reward staff members who excel in patient care and telemedicine adoption. Positive reinforcement can help boost the entire team’s morale and encourage them to be more enthusiastic about embracing telemedicine.
7. Office continuous training and support
Provide ongoing training sessions so your staff members can stay up to date about new trends in telemedicine and improvements/updates in the telemedicine platform. Foster a supportive culture where team members feel comfortable voicing their concerns, asking questions, and sharing experiences to learn from one another.
Encourage collaboration and teamwork to enhance telemedicine practices further.
By following these actionable tips, you can train your staff and equip them with the necessary skills to use telemedicine effectively. Ultimately, this will lead to more optimal healthcare delivery and improved patient outcomes.
Wrapping Up
As we reach the end of this article, we’ve seen how telemedicine is a powerful tool that can be leveraged to enhance healthcare delivery, improving accessibility and reducing cost.
In this article, we have explored how to properly set up a successful telemedicine service, from identifying your objectives to optimizing telemedicine workflow to providing post-appointment follow-ups. We’ve also covered how to train your staff properly so they can utilize the platform optimally.
We hope this article has been helpful and you can use the information in this article to get started in setting up your telemedicine service.